How is Janani Suraksha Yojana performing in backward districts of India? – Part 1
14 February 2013
The Government of India (GoI) has ambitious plans “to transfer individual benefits from the Government directly into the bank accounts of beneficiaries”[1]. This has given rise to intense debates and discussions on direct cash transfers as a policy tool to administer social-welfare objectives of the government. Unfortunately, there has been a limited discussion of the evidence from cash transfer schemes currently in operation in India. This 4-part blog-post, based on a forthcoming working paper, partially fills this gap by analysing the performance of Janani Suraksha Yojana (JSY), a conditional cash transfer scheme aimed at promoting institutional delivery by providing money to women if they deliver in medical facilities. Incentives are also given to the local community health workers, Accredited Social Health Activists (ASHAs), if they facilitate such deliveries. The data for this exercise comes from PAHELI, a unique attempt to rapidly assess the status of human development, including maternal and child health, in some of the most backward districts in India (click here, here and here to know more about PAHELI)[2].
In part I, we discuss the JSY scheme and discuss whether it has been successful in increasing institutional deliveries. The section also briefly describes the PAHELI survey. In Parts II and III, we analyse specific indicators related to the JSY and ASHA. Our findings indicate that JSY is working reasonably well. Yet there are some concerns regarding delays in receiving payments and the limited role played by ASHAs in facilitating deliveries or making post-delivery visits. But the most important concern is the continued high proportion of women delivering at home. In Part IV, the blog series concludes with a discussion of a few possible reasons, which might prevent women from accessing government health facilities, drawing on existing literature.
About Janani Suraksha Yojana & PAHELI
Background
JSY is a flagship programme of the National Rural Health Mission (henceforth, NRHM), launched by the GoI in April 2005. The main objective of JSY is to decrease maternal and infant mortality by encouraging pregnant women to deliver in medical facilities[3]. This is sought to be achieved through the payment of a cash incentive to the woman if she delivers in a government medical facility or in an accredited private medical facility. As per the current eligibility criteria, any woman from the low performing States (LPS), irrespective of poverty status, number of births and age is eligible for these cash incentives, while in the high performing States (HPS), a woman has to be above 19 years of age and below the poverty line[4]. The amounts of incentives are shown in table 1.
Table 1. Current Incentives under JSY (in Rs.)
| Amount of Incentives (Rs.) | ||
| State category | Rural area | Urban area |
| Low Performing State (LPS) | 1400 | 1000 |
| High Performing State (HPS) | 700 | 600 |
In addition to facilitating demand directly by the beneficiary, JSY also introduced the Accredited Social Health Activist (ASHA), a trained female community health activist. Selected from the village itself and accountable to it, ASHAs are supposed to work as an interface between the community and the public health system, and play an important role in the context of maternal and child health[5]. As far as JSY is concerned, she is supposed to facilitate delivery in a government or an accredited private medical facility. As per the guidelines, she is to be paid Rs. 600 per delivery in government facilities in LPS and Rs. 200 in HPS[6].
Has the Scheme worked?
Figure 1 indicates that institutional deliveries have increased more rapidly in LPS post-2005, as compared to the HPS, and as a result, the gap between the two has almost disappeared. Figure 2 shows that the proportion of JSY beneficiaries has also shot up dramatically in LPS[7]. Rigorous evaluations using various rounds of nationally representative data sets suggest that JSY has contributed to this narrowing of the gap[8]. A number of qualitative studies and reports also indicate that JSY has played an important role in improving institutional deliveries[9].
Figure 1. Number of institutional deliveries in LPS and HPS[10]
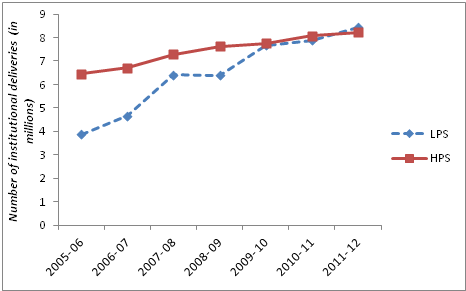
Source: NRHM (2012)
Figure 2. % of JSY beneficiaries after institutional delivery in LPS and HPS
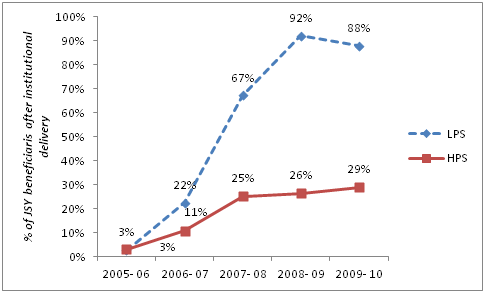
Source: NRHM (2012), RTIs filed by Accountability Initiative
It is in the backdrop of these impressive aggregate numbers that PAHELI offered us an opportunity to assess how well JSY actually functions, in some of the most backward districts located in the LPS.
PAHELI
‘People’s Assessment of Health, Education and Livelihood’ (PAHELI) is a rapid assessment of the prevailing status of human development, covering four major sectors: life and livelihood, water & sanitation, maternal & child health, and education & literacy[11]. It comprises of a set of simple survey formats that can be used by citizens to track progress towards the ‘Millennium Development Goals’ (MDGs), as well as assess the progress towards national objectives of poverty reduction, social protection and development of human capabilities.
The PAHELI survey was carried out in eight districts spread across seven states – Udaipur and Bhilwara (Rajasthan), Gumla (Jharkhand), Hardoi (Uttar Pradesh), Korba (Chhattisgarh), Nalanda (Bihar), Rajgarh (Madhya Pradesh) and Sundargarh (Odisha) – in the second half of 2011. 60 villages were selected randomly from each district and 20 households were selected from each of these 60 villages. This gave us a sample of 1200 households per district.
The questionnaire related to maternal and child health consisted of a series of questions which enquired whether the female respondent has accessed health care facilities in the period before, during and after pregnancy; the role of health workers such as ASHA and Auxiliary Nurse Mid-Wife (ANM); and most importantly, whether the pregnant woman received benefits under JSY after delivery and what impediments, if any, were encountered while obtaining these benefits. These questions were asked only to those women who had a child in the age group of zero to three years as on the date of survey.
In the next part, i.e., Part II, we analyse the performance of the scheme with respect to some specific indicators such as the proportion of institutional deliveries out of total deliveries, receipt of cash benefits, mode of payment, amount received, etc.
[1] Press Information Bureau, Prime Minister sets up the Architecture for Cash Transfers, September 28, 2012
[2] Accountability Initiative was a knowledge partner in this exercise.
[3] Maternal deaths in India account for 19.5% of the global maternal deaths (See Trends in Maternal Mortality-1990 to 2010 for details). Though maternal mortality ratio (MMR) has declined from 254 in 2004-06 to 212 in 2007-09, it remains high (Office of Registrar General, 2011).
[4] Low performing States are the ones where the proportion of institutional delivery was very low at the start of the NRHM. These include Jammu & Kashmir, Himachal Pradesh, Uttaranchal, Uttar Pradesh, Bihar, Orissa, Jharkhand, Madhya Pradesh, Chhattisgarh, Rajasthan, Assam, Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura.
[5] http://mohfw.nic.in/NRHM/asha.htm#abt
[6] Some States have divided this amount into three components- Rs. 250 for transport, which is given to whoever pays for the transport (may not be ASHA), Rs. 200 as an incentive for ASHA (non-transferable) and Rs. 150 if ASHA escorts woman to the facility/ stays with her.
[7] The underlying data has been obtained from the NRHM documents and through the RTIs filed by Accountability Initiative.
[8] Lim et al., 2010; Dongre, 2012 (revised); Joshi & Sivaram, 2012 (personal communication)
[9] CORT, 2007; UNFPA, 2009; NHSRC, 2011; NRHM, 2011
[10] The States in North-East and Union Territories are excluded in these calculations.
[11] See PAHELI Report (ASER et al., 2012) for details (http://www.asercentre.org/Keywords/p/63.html).





