
India’s stunted progress on child health
1 January 1970
How far has India progressed on securing welfare of all? This blog is part of a series which uses data to unpack the status of health, education and policy reforms in India’s 71st year of freedom.
Despite nearly 71 years of independence, children are still bound by malnutrition and poor health, a result of absolute poverty and an ineffective state. It is widely recognised that health issues from nutritional deficiencies in childhood can have a compounding effect in adult life. Inadequate healthcare can be debilitating to society at large from multiple vantage points: public participation, individual freedom, and labour supply. Healthier citizens are more able to participate in public life and public activities, can choose from a larger set of opportunities, and are more capable in their jobs. Simply put, healthier individuals are able to do more, be more, and contribute more (for more on this see my colleague Avani Kapur’s piece). A critical question stares us in the face at this juncture: what is the actual status of child health in India?
Dire Straits for Children
There are several indicators that reflect the long-term health and nutritional experience of an individual or population. One can check whether a child is stunted, underweight, or wasted[1]. Studies have linked stunting to lower cognitive development, among other unfavourable outcomes. Stunting is caused by long-term insufficient nutrient intake and frequent infections, and the effects are largely irreversible. In addition, cognitive development is also impaired by anaemia (low haemoglobin caused by iron deficiency). Wasting is a result of acute significant food shortage and/or disease, and is a strong predictor of under 5 mortality. Figures reveal that over 16 per cent of children in India are severely stunted, as many as 58 per cent children are anaemic, while close to 7 per cent are severely wasted.
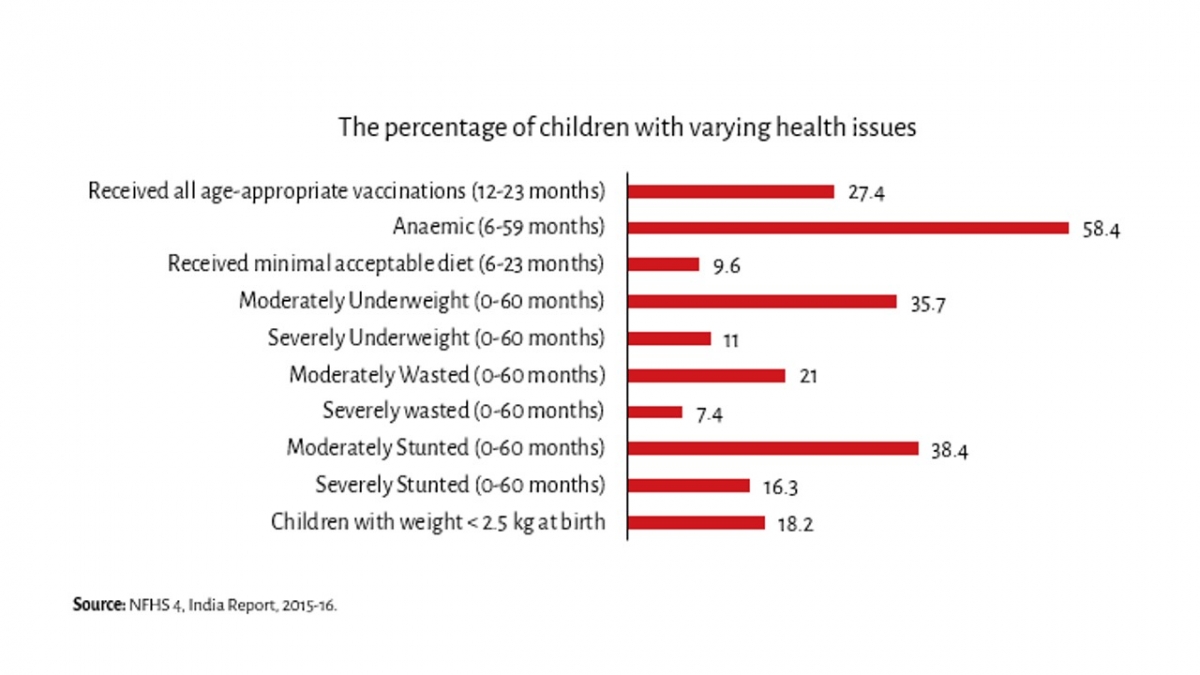
These poor outcomes are in part, borne of inadequate diets – less than 10 per cent children (6-23 months) receive the minimum acceptable diet[2]. Starvation deaths still occur, as sheer poverty and deprivation has precluded a large number of people from being able to feed themselves or their children restricting their future lives. Age-appropriate vaccination[3] coverage also remains low (27.4 per cent), thereby compounding the magnitude of the health problem. The state of child health in India is grave. Successive governments have recognised this and put into action various programmes to tackle the issue.
Anganwadi Centres are vital, but fall short of requirements
The Poshan Abhiyaan (National Nutrition Mission), launched in March 2018, has been one such step and aims to address malnutrition through convergence across ministries, improved technology, and better targeting. It is premature to know of its impact, yet, critical in the battle against malnutrition have been Anganwadi Centres (AWCs) under the longstanding (since 1975) Integrated Child Development Services (ICDS) programme. As part of the programme, children and lactating and pregnant mothers have been eligible to cooked meals, health check-ups, and immunisation services.
Even today, AWCs do not cover all children who require these services: only 1 in 2 children received any service according to NFHS 4 data. A quarter of ICDS beneficiaries are malnourished, a number that has increased from 15 per cent in 2015 to 25 per cent in 2017, as per analysis by the Accountability Initiative. This shows that even as ICDS coverage is expanding to include those who need it most, malnutrition remains a problem among those that avail ICDS services.
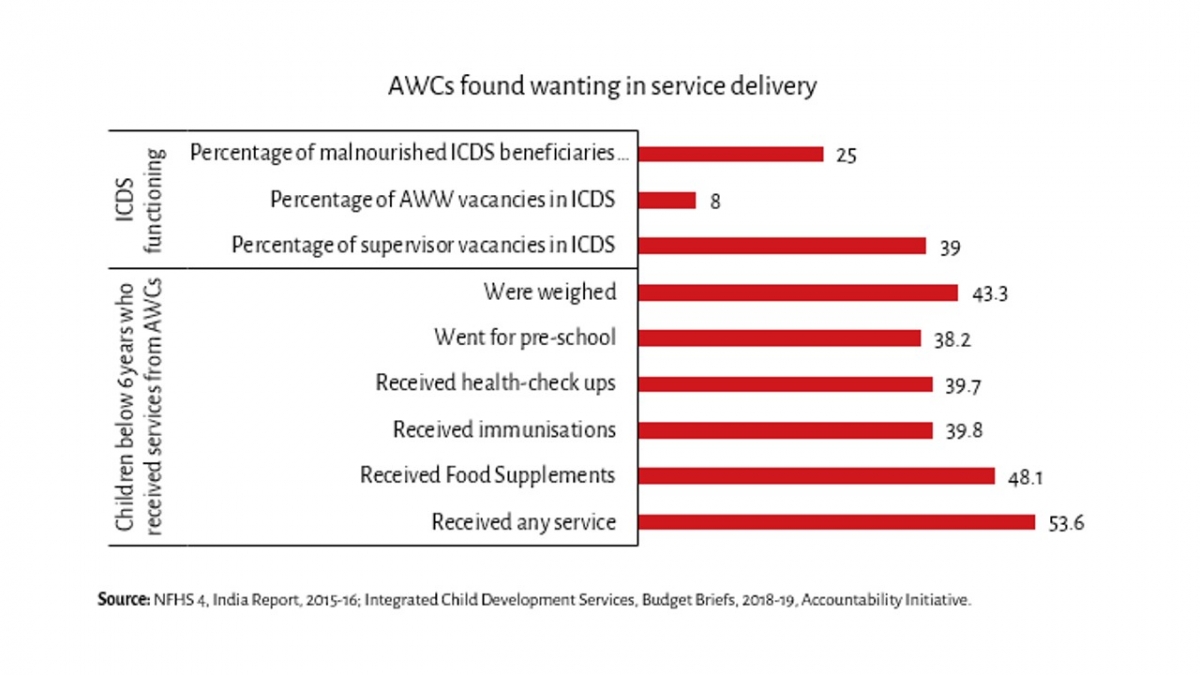
The quality of services provided continues to be weak. Out of ICDS beneficiaries, less than half received food supplements in 2015-16. Only 70 per cent Anganwadis had drinking water facilities, and 63 per cent AWCs had toilets.
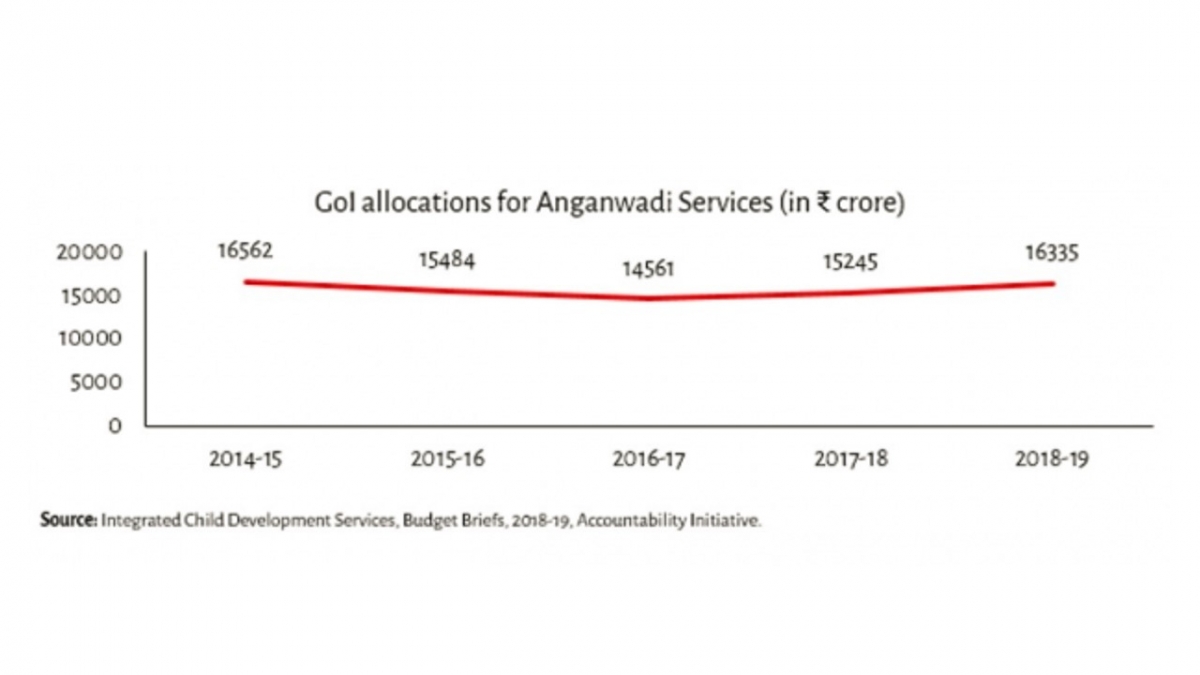
In light of such deficiencies, funding by the government is meagre. The government seems to have given short shrift to increasing the amount spent on child health, which has remained stagnant for successive years. Expenditure on supplementary nutrition declined by 6 per cent between 2015-16 and 2016-17. Anganwadi workers and helpers are still treated as ‘honorary workers’, and are paid a lean amount (approximately ₹5,100 and ₹2,820 respectively, on average), unadjusted for inflation. Furthermore, they are not entitled to minimum wages, according to the government. For the amount of work, and the skill required, such low pay can be distressing and as a consequence has led to strikes by workers time and again in various states to demand better pay. Additionally, of all sanctioned posts for Anganwadi workers, 8 per cent were vacant, as on March 2017. Vacancies are even higher among supervisors, which weaken monitoring, implying that even fully functional AWCs may not run efficiently.
Since the Anganwadi system is a critical asset in the fight against malnutrition, what are the consequences of these lapses for the poor, who critically depend on public health programmes?
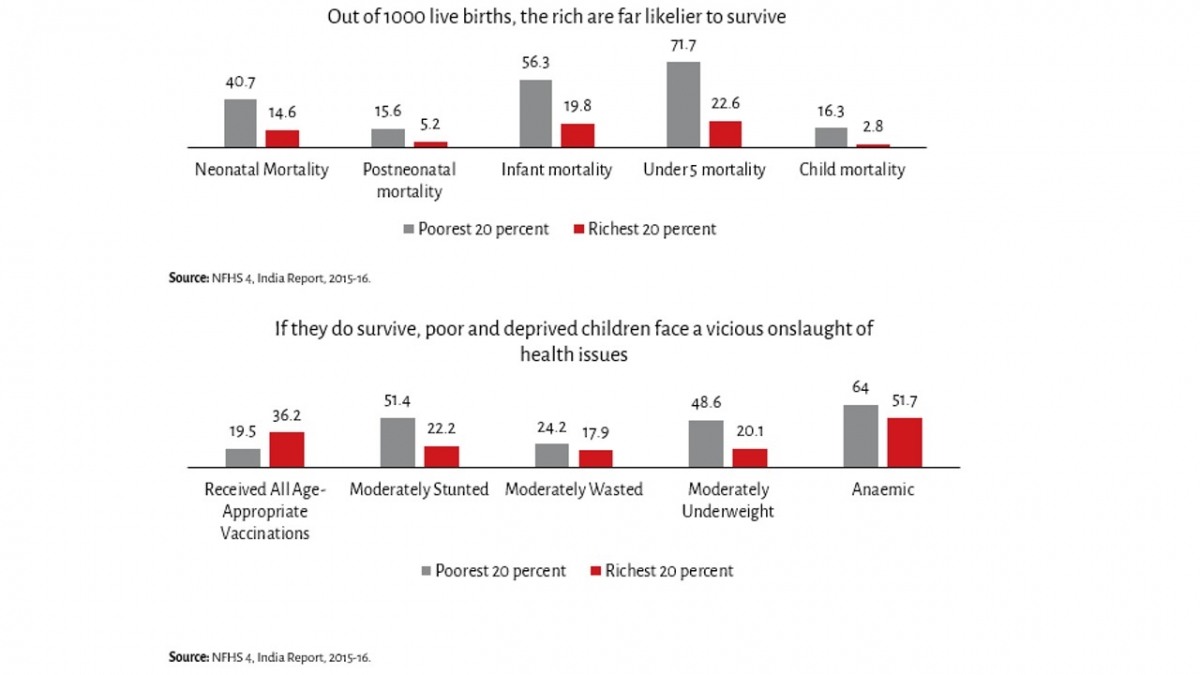
Wealth IS health, in most cases
There is stark inequality in how children of the poor and rich survive. Out of 1,000 live births, 72 infants of the least wealthy 20 per cent don’t survive until their fifth birthday, compared to 23 for the wealthiest. For those among the poorest and worst off who do survive, more than half are stunted, and almost half are underweight. Clearly, poor and deprived children are worse off than their richer counterparts. These inequalities continue to persist later in life and affect educational and occupational opportunities, and aggressively exacerbate income and wealth inequalities even further.
The rich and privileged don’t have to depend on weak public services, and have the resources and social capital to afford quality healthcare in private hospitals, which are out of the reach of the unprivileged. The wealthiest 20 per cent can afford better healthcare than the least wealthy. This seems to be true across several indicators – from access to vaccinations, to malnutrition and mortality rates at various stages of childhood.
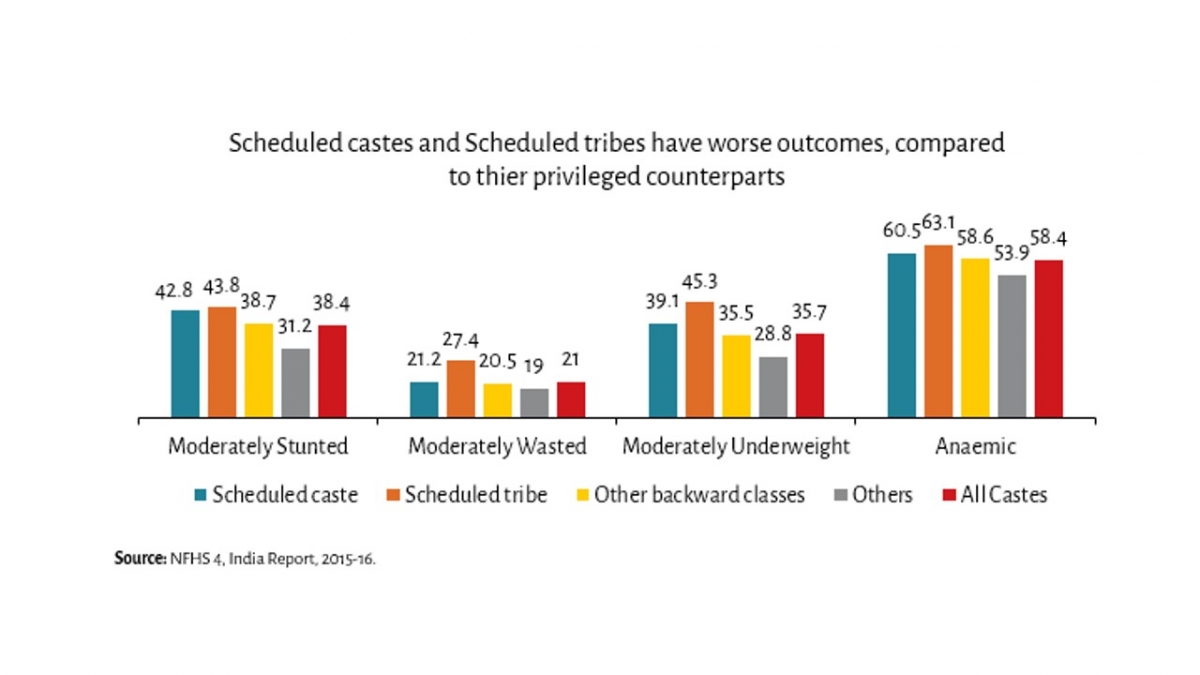
However, inequalities are not limited to wealth, or income. Caste and gender marginalisation persist in society, and these reflect in child health outcomes as well. Children of lower castes, or girls, face further issues due to their marginalisation by societies. Intersections of these inequalities adds to an already complex problem.
Sluggish improvement in outcomes: Does time heal all wounds?
A look at data from the last two decades reveals the extent of the progress the country has made. Over time, especially after India liberalised its economy in 1991, the quantity and quality of services provided has improved. However, progress isn’t as smooth as one would expect. Malnutrition has reduced, but not on all indicators. There has been a 10 percentage point reduction in stunting in the decade before 2015-16. However, every 2nd child is anaemic, and the propensity of wasting has actually increased.
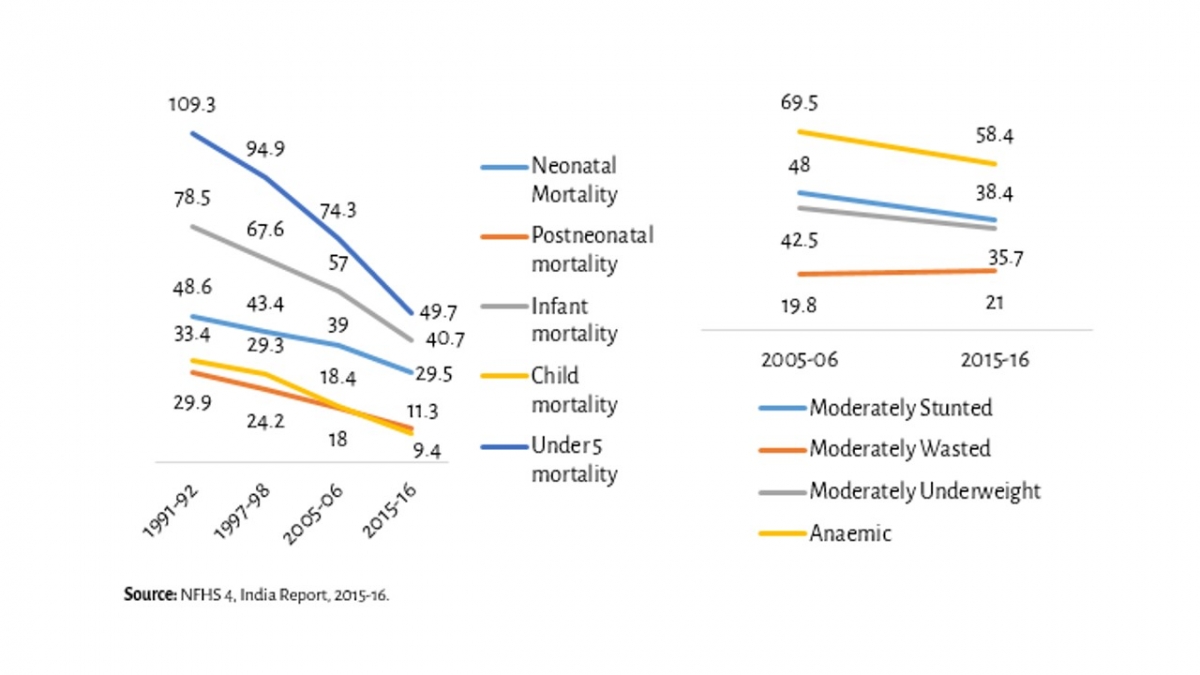
Compared to malnutrition, there has been marginally better progress in the survival rates of children. At the same time, under 5 mortality still remains very large. Of every 1,000 children born, 30 do not live beyond a month, about 41 do not live beyond a year, and about 50 children will die from birth till their 5th birthday.
It is thus clear that despite several government programmes, including the presence of ICDS since 1975, severe malnutrition in childhood has persisted over time, and is much worse for the poor and unprivileged sections of society. This has clearly restricted people from rising up the income and wealth scale, and the impact in time and money lost on private spending due to weak public nutrition services that should be easily accessible, is incalculable. The current government has responded with recent programmes like the Poshan Abhiyaan and the Rashtriya Swasthya Bima Yojana. The former includes a slew of activities involving at least 10 Union ministries and components as diverse as medical intervention, behaviour change, capacity building of frontline workers, and technological innovations, among others. The latter seeks to improve access to healthcare by providing insurance. Moreover, the renewed focus on sanitation is a welcome step. The hope, somewhat ambitiously, is to reduce stunting from 2 in 5 children to 1 in 4 children by 2022. The question is, will the government’s efforts be able to mend lapses of the past, and set the system on rapid course correction?
Inputs by Avantika Shrivastava
India increasingly faces dual burden of malnourishment: under-nourishment & over-nourishment. While 2/10 people are thin, 2/10 are overweight. Know about this emerging challenge to the public health system in the second part of this series.
[1] Stunting refers to low height-for-age, being underweight refers to low weight-for-age, and wasting refers to low weight-for-height. Moderate and severe malnourishment refer to people below two and three standard deviations below the normal, respectively.
[2] 4+ food groups, breastmilk, other milk products, and are fed with appropriate frequency.
[3] BCG, measles, four doses of hepatitis B, and three doses each of DPT and polio vaccine (excluding polio vaccine given at birth)





